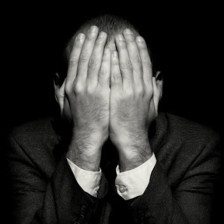
The voice of grief is rather convincing, isn’t it?
It tells you you’re “too old,” “not good enough,” or “not worthy enough” for another chance at life, that starting over is impossible.
This voice in your head is the first thing you hear in the morning and the last thing you hear at night. It drives with you to work. It stays with you at lunch.
Its message is so consistent that, because of its repetitive power, you may be inclined to believe it. But, as persuasive as the voice of grief is, everything it says is a lie.
It’s all a pack of lies.
Do you want the truth?
If you do, then start listening to life calling to you inside your grief.
How?
Every time you are yearning to be held and loved, to laugh again, listen to your yearning.
Do not listen to your fear.
Listen to life calling you:
- I am here, come on over.
- Take a chance on me.
- I am your life, and you’re all that I’ve got.