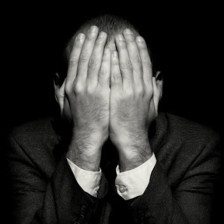
No Matter what I do it is there, it is always there, it is prodding me, poking me, tormenting me.
“It” whatever “it” is has stolen my life.
And you don’t deserve to have it. Who are you anyway and where did you come from?
I am not sure I was ever whole, but how dare you relegate me to the sidelines.
How dare you have the audacity to think you run things here.
This is my life, and you, “it” can go fuck yourself.
I will call you BDD because that is the name they give you.
Honestly, it doesn’t really matter to me, you are just an evil mother fucker in my book who has stolen my life from me.
Yours, is a self conscious, ego-centric world that I don’t live in.
But you have cuffed me and chained me to this.
You are my abuser that I can’t let go of.
And I keep coming back for more.



![Forceful Feelings [1]](https://i0.wp.com/farm4.staticflickr.com/3445/4601905733_5b33886003_z.jpg?resize=600%2C390)

