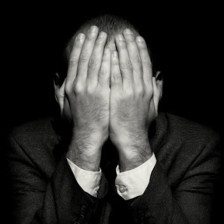
I have Body dysmorphic disorder
There has always been something wrong with my face.
There was a time when I’d be able to sit in front of a mirror for hours on end and make note of every imperfection I could find.
- My nose was too big.
- My eyes were too small.
- I’d look at magazines and think, “I want to be like this. I want to be tall and skinny and white.”
- “I want to be beautiful.”
Every night before I went to bed, I’d pray to God or whatever entity out there to please, please make me pretty.
I AM OBSESSED
I have literally found myself wishing there would be a SARS outbreak in my city just so face masks would be necessary.
I am not formally diagnosed with BDD, but I know this is what I have.
The reason why I’m reluctant to talk to any professionals with experience on the matter is because I know they will keep me from saving myself.
They’ll take away the possibility of surgery.
For the past five years, I have been infatuated with aesthetic surgery and, as sad as this may sound, still perceive it as a form, or rather, my form of salvation.
I am self-conscious to the extent of covering my face with a post-it during a webcam session.
In person, my attempts to hide my “mug” aren’t as effective, but they still manage to be noticeable. And even with that said, I really, really am trying to be inconspicuous. I really am trying to stop.
I honestly don’t understand why I’m like this, but I do know that it’s not for the validation of other people.
I can give a flying **** about compliments. Sure, they may make me feel a bit better for the time being, but they ultimately won’t change a thing. I do realize that I’m not insanely hideous, I just… can’t help it. It’s weird.
A SILLY STORY
When I was little, maybe five or so, I was peering in the mirror when I noticed that my lips were huge.
This irked me so much that I proceeded to grab a pair of scissors and cut small pieces of it off until I was satisfied. There was no pain, just this numbness and a feeling of contentment.
An hour later, it hurt, BAD!
Now, why do I hide these “huge” lips?
First thing’s first: The bane of my existence is my lack of self-esteem. The cause of that, contrary to popular belief, isn’t my lips. The cause is, in fact, my nose. I am so deluded that I blame and associate some of my mistakes to my nose, and sometimes, I veritably believe it.
They say the first step is recognizing the problem, right?
It’s a shame I haven’t looked much into the whole procedure.
Anyway, suck in your lips for a moment. If you look in the mirror while doing this, you can see that it slightly alters the shape of your nose. This is why I do it. Because I’m convinced my nose looks a bit better with my lips sucked in.
ON REFLECTION – I AM CRAZY
The first thing I am going to do once I get out of high school is to go to Korea or Japan for a nose job. Then, maybe these stupid psychological issues won’t deter me from living life to its full extent. This, I genuinely believe, and I am more than willing to take a risk to ensure it.
You’re probably wondering what will I do if surgery doesn’t work out.
And to be honest, I don’t know either. I try not to dwell on it as an attempt to preserve all the optimism I currently have left.
– If Only