We all wish for our kids to be strong, confident men and women.
We would tell them that they should respect and care about their bodies.
We would tell them to listen to their hearts, to be who they are, to not let the world dictate their decisions, or make them into something they aren’t.
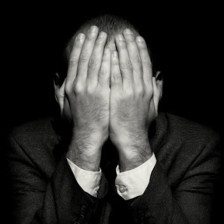
Yet those of us with BDD are just the opposite.
We let the world dictate our day, we let the feelings of the thoughts of others make us who we are.
If we believe the world thinks we are monsters, then that is what we are, monsters.
We want our kids to live a different life.
My kids don’t know I have BDD, and it is my goal to make sure they never do.
It is not because I don’t want to tell them, because I do.
It is not because I want to protect them, because I know they can handle any truth.
It is because I want them to grow up respecting themselves.
I don’t want them to live in fear like their dad.
I want them to stand in front of the mirror and be proud of who they are.
I want them to know that they can be anything they see (or can imagine) in the world.
I want them to stand confident and proud.
I want them to be who I know I could be if I didn’t have BDD.
A man lost inside his mind, letting the world dictate who he is, afraid of his shadow, walking a fine line between sane and insane.
What would I do if my kids had BDD?
I would tell them they should love themselves as they are… perfect creations of God. Beautiful in every sense of the word.
So, no I am not going to tell my kids I have BDD.
I am instead going to overcome it, and in doing so I am going to tell (show) them a truth that all of us with BDD know deep in side but just can’t accept:
That we are “good enough”, we are just what we need to be, perfection is a lousy lot, we are beautiful, strong and capable human beings. Filled with love and compassion, here to have an experience of life.
Life if so fleeting, so impermanent, so precious. Let us not waste it on self pity and shame.
To send a different message to my kids would be to steel their time.
Don’t tell your kids you have BDD, instead tell them you love them and then show them the way you want them to be.